You are here
Content
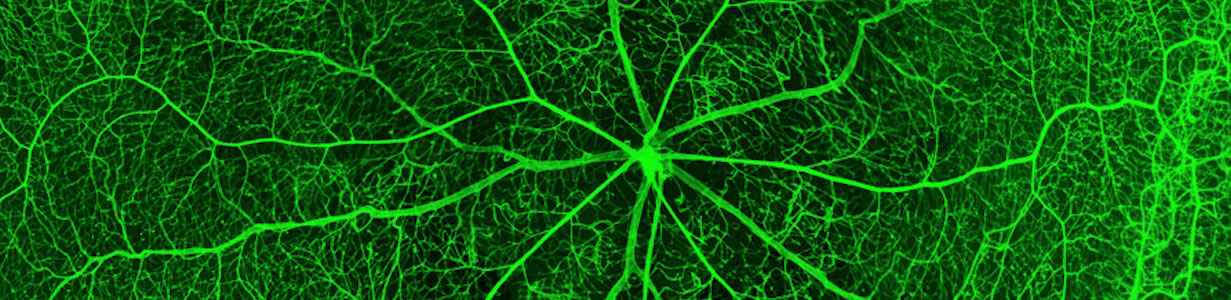
The blood supply of all organs has to be adjusted to different and permanently changing conditions at any time. However, adequate matching of blood supply to actual demand is often disturbed, in particular in widespread diseases of the circulatory system like hypertension and diabetes. Therefore, the mechanisms regulating blood supply are still an area of active research.
In the Division of Cardiovascular Physiology we are investigating the role of different signaling molecules, in particular ion channels, in vascular smooth muscle cells and of mechanically induced signaling cascades in endothelial cells of different vascular beds. Special attention is paid to physiological regulation (myogenic and perivascular-fat dependent autoregulation, mechanical stimulus-induced signaling, functional remodeling of the vascular wall) and related pathophysiological processes (diabetes, hypertension, atherosclerosis). A broad spectrum of methods from the molecular and the cellular level up to the level of intact organs is employed.
Three main topics are studied:
- The role of vascular smooth muscle potassium channels in mechanisms of autoregulation of the circulatory system under physiological and pathophysiological conditions
- The mechanisms of functional and structural plasticity of the vascular wall in response to mechanical stimuli and during postnatal development
- The role of endothelial glycocalyx in pathological conditions like inflammation, thrombosis and atherogenesis
It is our long lasting goal to get a comprehensive understanding about the function of different signaling molecules as members of larger signaling complexes and about the regulation of their function at the subcellular level. This will enable us to delineate acute autoregulatory as well as long lasting functional remodeling processes in the circulatory system under physiological and pathophysiological conditions.
Project-related publications
- Gaynullina D, Dweep H, Gloe T, Tarasova OS, Sticht C, Gretz N, Schubert R: Alteration of mRNA and microRNA expression profiles in rat muscular type vasculature in early postnatal development. Sci Rep. 5: 11106 (2015) doi: 10.1038/srep11106
- Gaynullina D, Lubomirov LT, Sofronova SI, Kalenchuk VU, Gloe T, Pfitzer G, Tarasova OS, Schubert R: Functional remodelling of arterial endothelium during early postnatal development in rats. Cardiovasc Res, 99: 612-21, 2013.
- Zavaritskaya O, Zhuravleva N, Schleifenbaum J, Gloe T, Devermann L, Kluge R, Mladenov M, Frey M, Gagov H, Fésüs G, Gollasch M, Schubert R: Role of KCNQ Channels in Skeletal Muscle Arteries and Periadventitial Vascular Dysfunction. Hypertension, 61: 151-9, 2013.
- Lidington D, Schubert R, Bolz SS: Capitalizing on diversity: an integrative approach towards the multiplicity of cellular mechanisms underlying myogenic responsiveness. Cardiovasc Res, 97: 404-12, 2013.
- Dreher L, Elvers-Hornung S, Brinkmann I, Huck V, Henschler R, Gloe T, Klüter H, Bieback K: Cultivation in Human Serum Reduces Adipose Tissue-Derived Mesenchymal Stromal Cell Adhesion to Laminin and Endothelium and Reduces Capillary Entrapment. Stem Cells Dev, 22: 791-803, 2013.
- Bieback K, Vinci M, Elvers-Hornung S, Bartol A, Gloe T, Czabanka M, Klüter H, Augustin H, Vajkoczy P: Recruitment of human cord blood-derived endothelial colony-forming cells to sites of tumor angiogenesis. Cytotherapy, 15: 726-39, 2013.
- Hennig T, Mogensen C, Kirsch J, Pohl U, Gloe T: Shear stress induces the release of an endothelial elastase: role in integrin a(v)ß(3)-mediated FGF-2 release. J Vasc Res, 48: 453-64, 2011.
- Mogensen C, Bergner B, Wallner S, Ritter A, d'Avis S, Ninichuk V, Kameritsch P, Gloe T, Nagel W, Pohl U: Isolation and functional characterization of pericytes derived from hamster skeletal muscle. Acta Physiol, 201: 413-26, 2011.
- Schleifenbaum J, Köhn C, Voblova N, Dubrovska G, Zavarirskaya O, Gloe T, Crean CS, Luft FC, Huang Y, Schubert R, Gollasch M: Systemic peripheral artery relaxation by KCNQ channel openers and hydrogen sulfide. J Hypertens, 28: 1875-82, 2010.
Context Column
Contact

Prof. Dr. Rudolf Schubert
Cardiovascular Physiology
Center for Biomedicine and Medical Technology Mannheim (CBTM)
Medical Faculty Mannheim
Heidelberg University
Ludolf-Krehl-Str. 13-17
68167 Mannheim
Phone +49 621 383-9640
rudolf.schubert@medma.uni-heidelberg.de