Sie befinden sich hier
Inhalt
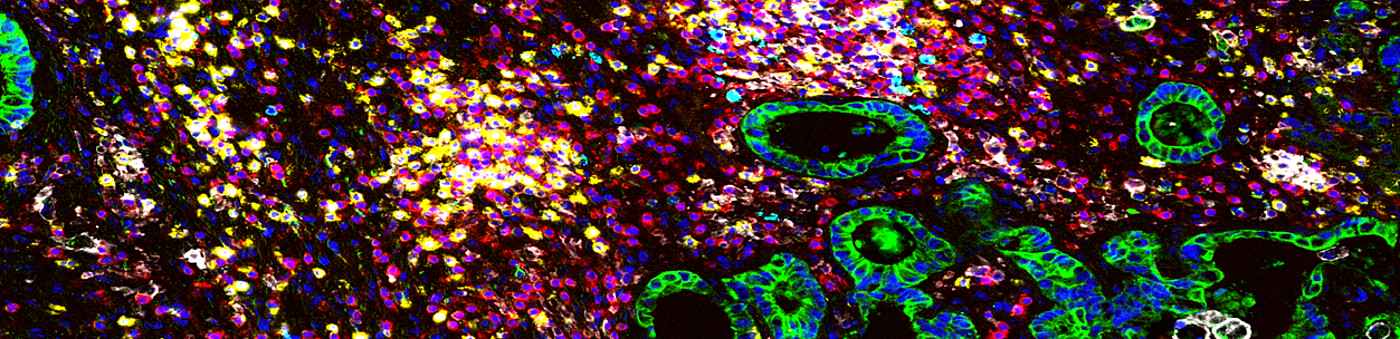
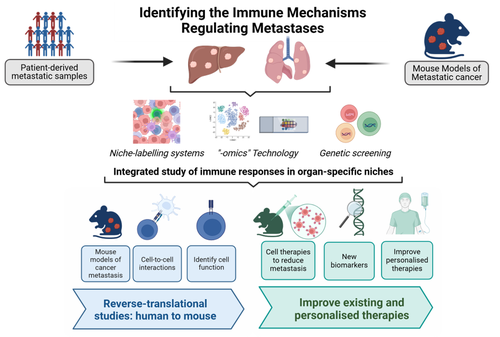
In our lab, we study immune mechanisms regulating metastatic disease, focusing on:
- Regulation of innate lymphoid cell function in metastasis, tissue damage and repair
- Tissue-specific features of innate lymphocytes
- The role of memory T lymphocytes in anti-metastatic immunity
- T lymphocyte-myeloid cell Interactions in metastasis
- Immune niches linked to therapeutic response and prognosis in metastatic disease
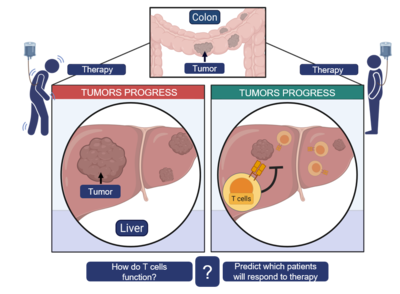
Liver metastasis:
Improving chemotherapy outcomes and relapse
Colorectal cancer (CRC) frequently advances to colorectal liver metastasis (CRLM), where patient outcomes remain variable despite improvements in treatment. While neoadjuvant therapy can increase resectability and improve prognosis, many patients show limited response, and recurrence after resection is common. Our research focuses on understanding the immune landscape of CRLM, particularly the roles and spatial dynamics of T cell–myeloid cell interactions within the tumor microenvironment. The goal is to uncover mechanisms that shape clinical outcomes and inform future therapeutic strategies.
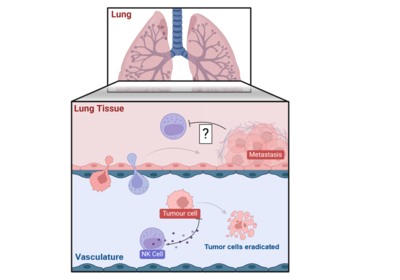
Lung metastasis:
Unlocking NK cell potential in immunotherapy
The lung is a common site of metastatic spread, where immune surveillance by Natural Killer (NK) cells plays a critical protective role. Despite their cytotoxic potential, NK cells are often rendered ineffective within the metastatic microenvironment, allowing tumor cells to evade immune elimination. Our research has identified distinct NK cell subsets residing in the vasculature and metastatic lesions, some of which retain the capacity to eliminate tumor cells. This project aims to dissect the mechanisms driving NK cell dysfunction in lung metastases and to develop strategies that restore and enhance NK cell cytotoxicity for therapeutic application.