Sie befinden sich hier
Inhalt
Non-constrast enhanced MRI of lung perfusion and ventilation by Fourier Decomposition
G. Bauman1, M. Puderbach2, M. Deimling3, V. Jellus3, C. Chefd'hotel4, H-U. Kauczor5, L. Schad6
Introduction
Evaluation of regional pulmonary perfusion and ventilation has important clinical value as an indicator of lung function. Current standard MR based methods for assessment of lung perfusion and ventilation are dependent on the application of the inhalative or the intravenous contrast agents. We propose a Fourier Decomposition method for non-contrast enhanced functional lung MRI [1]. The method was adapted on a 1.5 T clinical MR scanner using fast acquisition and submillisecond echo sampling with an optimized Steady-State Free Precession (SSFP) sequence to produce time-resolved 2D data stacks [2]. Application of Fourier analysis of the data along the temporal dimension allowed for spectral separation of the signal changes caused by lung parenchyma contraction and blood pulsation. The goal of this study was to verify the technical and medical reproducibility of the Fourier Decomposition method in a volunteer population.
Methods
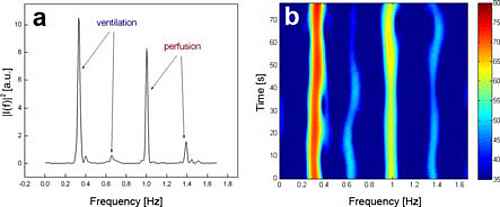
All measurements were performed on a 1.5 T MR whole body scanner (Siemens MAGNETOM Avanto, Erlangen, Germany) using a 12-channel thorax/spine coil as the receiver and transmitter. Twelve healthy volunteers (nine men and three women) with mean age of 31.5 ± 12.1 years (range = 19 - 61 years) were examined. A set of six coronal slices was acquired using time-resolved scans with a SSFP sequence to partially cover the volume of the chest. The identical measurement protocol was repeated after 24 hours in every subject. The imaging parameters were: TR = 1.9 ms, TE = 0.8 ms, α = 75°, slice thickness = 15 mm, FOV = 450² mm², matrix 96 x 128 zero-filled to 256 x 256, TA = 0.11 s per image. Time-resolved set of n = 198 images was acquired for every slice with a total acquisition time T = 59.4 s, spectral resolution Δf = 1/T = 0.017 Hz and spectral width fB = 1/(2⋅TA) = 1.667 Hz. Neither a breath-holding nor ECG triggering were required. Each image within every data stack containing single slice was corrected for the respiratory motion using a nonrigid registration algorithm with respect to a chosen reference image [3]. Pixel-wise application of Fourier Transform along the time axis of the data sets converted them into stacks of n images representing spectral frequencies fn ∈ {0, Δf, ... , fB}. Periodical signal intensity changes with regard to the cardiac and respiratory cycles were identified on a frequency spectrum (see Fig. 1a). Stability of both physiological cycles during a measurement was shown on a short-time Fourier Transform spectrogram in Fig. 1b. Since the time course was non-sinusoidal, second harmonic frequencies for respiratory and cardiac cycles were observed in the spectrum. After an integration of appropriate spectral ranges perfusion and parenchyma density maps were produced for every slice.
Results
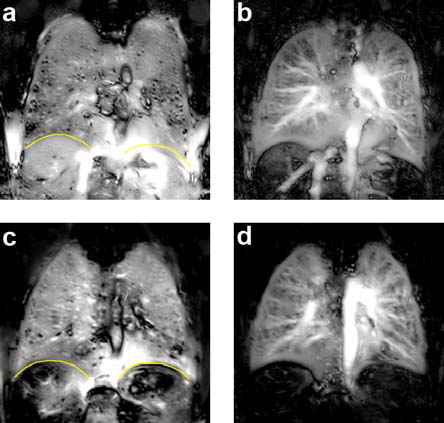
Four regions of interest were placed in the lung parenchyma (upper and lower lobes of both lungs) for every image. Signal intensity changes caused by respiration in time-resolved data sets was 15.1 ± 4.6 % and by blood pulsation 7.3 ± 1.8 %. Average signal to noise ratio (SNR) for perfusion maps was 95.1 ± 13.6 and for ventilation maps 213.9 ± 88.3. Example parenchyma density and perfusion maps are shown in figure 2. SNR averaged in registered images for all subjects was 26.9 ± 5.3. Effect of gravitational forces on the distribution of the stationary blood in the lung tissue for the supine body position was observed [4]. The most dorsal slice showed SNR of 31.6 ± 9.7 and the most ventral of 22.8 ± 4.2. Signal intensity was related to the dorsal-ventral direction with a mean slope of -3.9 ± 1.3 %/cm. The SNR in perfusion maps was proportional to the amplitude of signal changes with regard to the blood pulsation and was not statistically dependent on the dorsal-ventral direction. In case of ventilation maps there was significant change of SNR in the dorsal-ventral direction of -9.2 ± 5.4 %/cm.
Discussion
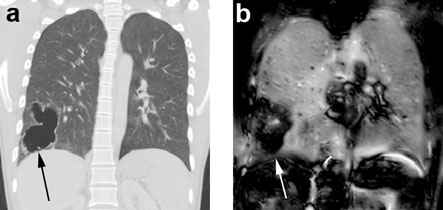
The study shows the feasibility of the Fourier Decomposition method to obtain perfusion and ventilation related information in a volunteer population. Neither administration of intravenous contrast agents nor inhalative gaseous media like hyperpolarized helium [5], oxygen [6] is needed. The mean slope value describing the gravitational effect of the distribution of the signal intensity in the lung parenchyma was found to be close to the data published by Hopkins et al. [4]. Although there is a spectrum of image quality in the group of volunteers, even “poor quality images” seem to be of diagnostic value. Images obtained from a patient with a cystic parenchymal defect in figure 3 show hints towards the clinical feasibility of the Fourier Decomposition method. The presented method requires only minimal patient compliance and is not dependent on triggering techniques. It could be an alternative approach for functional lung assessment using MRI. Further clinical studies in patients with lung diseases are needed to validate the clinical impact of the proposed method.
1 Medical Physics in Radiology, German Cancer Research Center, Heidelberg, Germany,
2 Department of Radiology, German Cancer Research Center, Heidelberg, Germany,
3 Siemens Healthcare, Erlangen, Germany,
4 Siemens Corporate Research, Princeton, NJ, United States,
5 Department of Diagnostic Radiology, University Hospital Heidelberg, Heidelberg, Germany,
6 Computer Assisted Clinical Medicine, University of Heidelberg, Mannheim, Germany
References
[1] Deimling M. et al. Proc. 16th annual meeting ISMRM, 2008, Toronto, Canada, p. 2639
[2] Bauman G. et al. 94th annual meeting RSNA, 2008, Chicago, USA, 6011732
[3] Chefd’hotel C. et al. VLSM'2001, ICCV Workshop, 2001, Vancouver, Canada
[4] Hopkins S.R. et al. J. Appl. Physiol., 2007; 103(1): 240-248
[5] De Lange E.E. et al. Radiology, 1999; 210: 851-857
[6] Edelman R.R. et al. Nat. Med., 1999; 2: 1236-1239