Sie befinden sich hier
Inhalt
L. R. Schad, M. Bock, J. Debus, G. Weisser, R. Engenhart, W. J. Lorenz.
Introduction
Since the pioneering work of Leksell in 1951 (1), radiosurgery has become the most effective radiotherapy for arteriovenous malformations (AVM). Radiosurgery describes stereotactically guided single high-dose irradiation with a steep dose gradient outside the target volume allowing application of high doses to the AVM without damage to the surrounding normal brain tissue. According to this features radiosurgery is an effective therapy for AVM leading to the development of linear accelerator based radiosurgical techniques at our institution in Heidelberg (2). In a previous paper we showed, that MR angiographic imaging data (MRA) provides a sensitive, non-invasive, 3D method for defining target volume, critical structures and for calculating precise dose distributions for radiosurgery of AVM, if the data are free of geometric distortion (3). A further improvement for defining the nidus of the lesion and for therapy control can be reached by combining these data with 3D velocity data.
Methods
Measurements were performed on a standard 1.5T clinical scanner (Siemens, Magnetom). The RF transmitting and receiving unit consists of a self-made linear polarised head coil with an inner diameter of 31 cm which fits very closely to the stereotactic localisation system. We used a 3D velocity-compensated FISP sequence with magnetisation transfer (MT) pulse and increasing flip angle (TONE). The sequence parameters a repetition time (TR) of 40 msec, an echo time (TE) of 7.7 msec, one acquisition, and a 256 x 256 image matrix with a 128 partition slab resulting in an effective voxel size of 1 mm3. In addition, 3D velocity measurement was performed with a 32 partition slab of 64 mm thickness using the phase-contrast (PC) method. Different materials (steel, aluminium, titanium, plastic, wood, ceramics) were used for the stereotactic localisation system and tested to mechanical stability and geometric MR image distortion.
Results
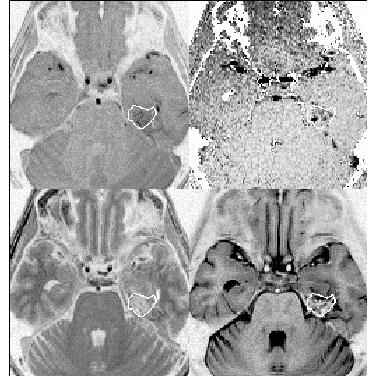
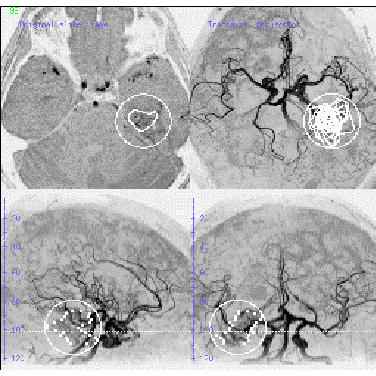
The definition of the target volume is shown in Fig. 1. The therapist can define the target volume either on the original (MRA, PC, T1-, or T2-weighted) images (Fig. 1a) or on maximum intensity projection (MIP) images at axial, sagittal, or frontal projections (Fig. 1b). After target volume definition the dose calculation can be performed on the basis of 3D MRA data. The 80 % isodose lines are indicated as circles in Fig. 1b. For each patient MRA was compared with available conventional brain angiograms. The AVM’s were assessed for the size of the nidus, the origin of the feeding arteries and the pattern of venous drainage. Since the patient's head was fixed in the same stereotactic localisation system for conventional angiography, the information about target volumes and target points could be precisely transferred from MRA to conventional angiograms for comparison. With the help of phantom measurements (3) it can be clearly demonstrated, that all stereotactic rings made of metal lead to a more or less dramatic geometric distortion and signal cancellation in the MR images. The best properties - no distortion together with a high mechanic stability - is given by the ceramic ring, which has to be carefully handled.
Conclusions
MRA and 3D flow measurements provide accurate 3D information about the anatomy and topography of AVM. Thereby the nidus of the lesions can be easily and precisely assessed on original images or on 3D angiographic projections which correlates well with conventional angiography in most of the cases. Because of the inherent risk and discomfort of repeated conventional angiographic examinations, MRA and 3D flow measurements are a useful method in our treatment protocol for planning of radiosurgery and follow-up of AVM for studying the dynamic process of obliteration after radiation.
References
[1] Leksell L. The stereotaxic method and radiosurgery of the brain. Acta Chir Scan 102:316-319;1951.
[2] Hartmann GH, Schlegel W, Sturm V, Kober B, Pastyr O, Lorenz WJ. Cerebral radiation surgery using moving field irradiation at a linear accelerator facility. J Radiation Oncology Biol Phys 11:1185-1192;1985.
[3] Schad LR, Ehricke HH, Wowra B, Layer G, Engenhart R, Kauczor HU, Zabel HJ, Brix G, Lorenz WJ. Correction of spatial distortion in magnetic resonance angiography for radiosurgical planning of cerebral arteriovenous malformations. Mag Res Imag 1992;10(4):609-621.